

To qualify for hospice care, patients must meet specific medical criteria indicating that their illness has reached a terminal stage. These guidelines ensure that patients receive comfort-focused care rather than curative treatments.
A life expectancy of six months or less, if the illness follows its natural course.
The prognosis must be certified by both the patient’s primary physician and the hospice medical director.
The patient elects to forgo curative treatments and chooses palliative care instead.
Hospice services may continue beyond six months if the patient continues to meet eligibility criteria.
Patients with advanced Alzheimer’s disease may qualify for hospice care when they meet both functional and clinical criteria, as outlined in the LCD (Local Coverage Determination) guidelines. Below is a comprehensive summary:
Have a life expectancy of 6 months or less, if the disease runs its normal course.
Having this prognosis certified by both the patient's primary physician and the hospice medical director
Choose to forego curative treatments
Continue to meet hospice criteria beyond 6 months if their condition continues to decline.
Eligibility typically begins at Stage 7 of the FAST Scale plus at least one significant complication or co-morbidity.
Here are the relevant FAST stages:
Difficulty putting clothes on properly
Inhability to bathe properly; may develop fear of bathing
Inhability to manage toileting
Urinary incontinence
Fecal incontinence
Speech limited to <6 intelligible words
Loss of all intelligible speech
Non-ambulatory without assistance
Unable to sit up independently
Unable to hold head up sit up independently

Aspiration pneumonia
Septicemia
Recurrent fevers despite antibiotics
Pyelonephritis
Multiple stage 3–4 pressure ulcers (decubitus)
Inability to maintain nutrition:
>10% weight loss in the last 6 months
BMI <18
Serum albumin <2.5 g/dl
Refusing to eat or difficulty swallowing
Weight loss despite artificial feeding (NG/G-tube, TPN)







ALS patients may qualify for hospice care when they meet specific criteria that reflect both their functional decline and clinical prognosis. Below are the guidelines for ALS patients:

Have a prognosis of 6 months or less to live if the disease progresses as expected.
Have this prognosis certified by both the patient’s primary physician and the hospice medical director.
Choose to discontinue curative treatments in favor of comfort care.
Hospice eligibility can extend beyond 6 months as long as the patient continues to meet eligibility criteria.
ALS patients may be considered for hospice if they are in a later stage of the disease with significant functional impairments, including:
Difficulty swallowing, speaking, and breathing.
Unable to walk or move independently without assistance.
Often indicated by a significant drop in body mass and difficulty maintaining nutrition.

Difficulty swallowing (dysphagia) and aspiration pneumonia
Severe malnutrition with >10% weight loss
Recurrent respiratory infections or pneumonia
Respiratory failure (requiring ventilator or bi-level positive airway pressure (BiPAP) support)
Progressive muscle weakness affecting limbs, neck, or diaphragm
Non-healing ulcers due to immobility





Onset of ALS symptoms: Duration and progression of muscle weakness
Current respiratory function: Use of respiratory support such as BiPAP or a ventilator
Speech and swallowing ability: Evidence of severe dysphagia and aspiration events
Mobility status: Bedbound or requiring significant assistance for movement
Weight loss: Documented >10% weight loss or inability to maintain adequate nutrition

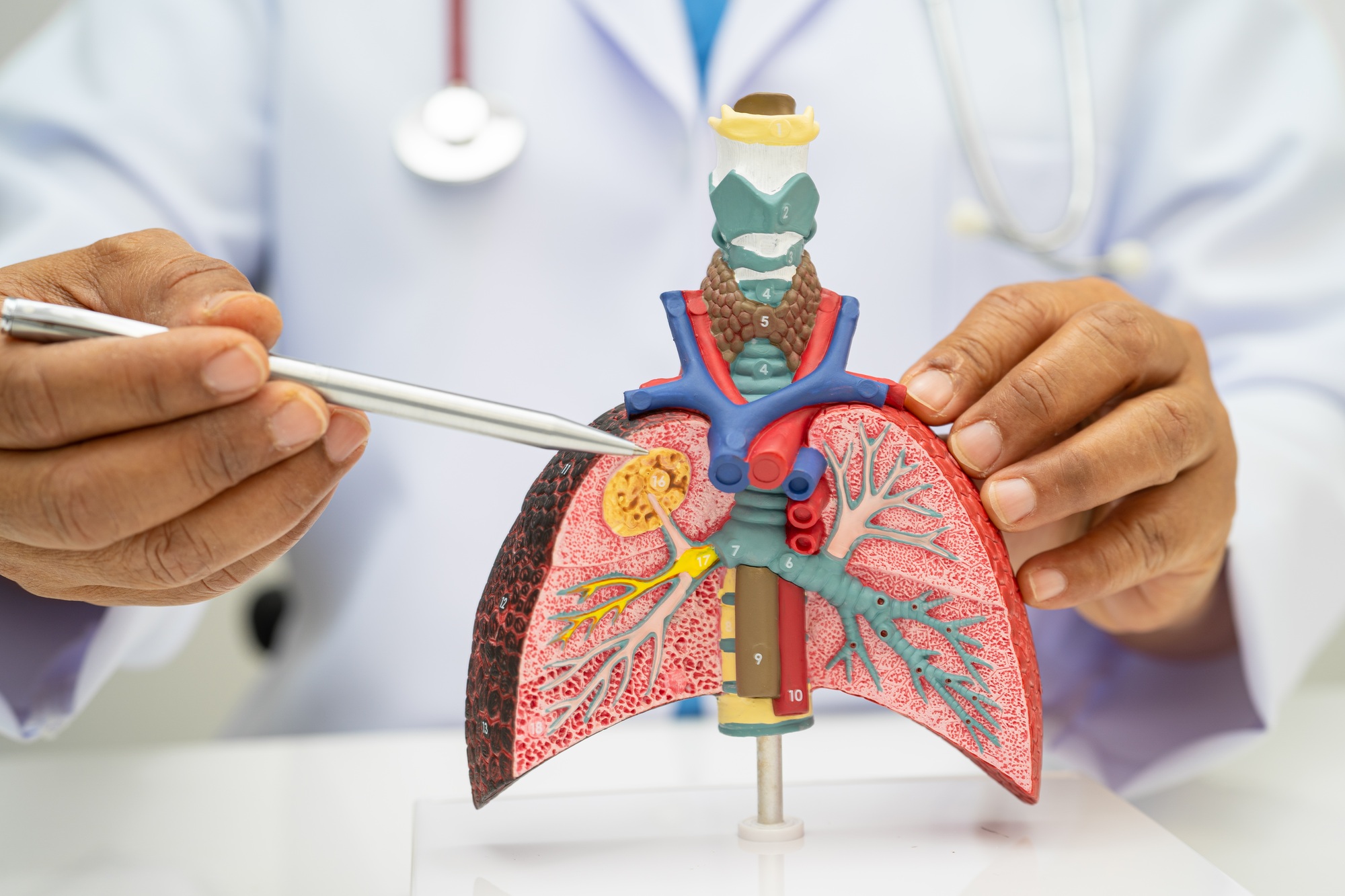
Patients suffering from severe pulmonary diseases may qualify for hospice care when they exhibit significant deterioration in their respiratory function and quality of life. The following criteria help identify eligibility for hospice:
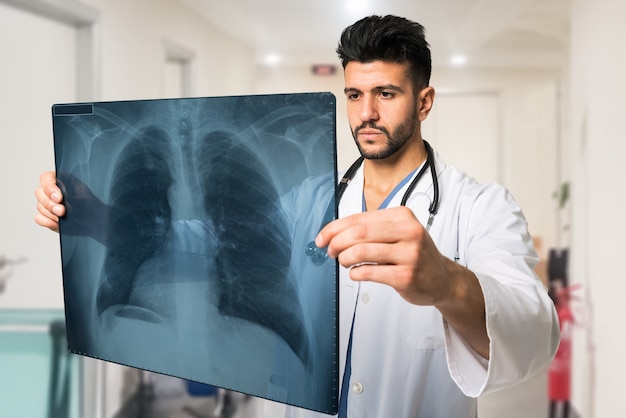
Have a prognosis of six months or less to live if the disease follows its normal course.
Have this prognosis certified by both the patient’s primary care physician and the hospice medical director.
Choose to forgo curative treatment in favor of comfort care.
Hospice eligibility may extend beyond six months if the patient continues to meet the necessary criteria.
Pulmonary disease patients may be eligible for hospice if they experience significant limitations in breathing and overall functionality, such as:
(dyspnea) even with minimal exertion.
for respiratory issues or complications, such as pneumonia or respiratory failure.
for most of the day, with reduced effectiveness in controlling symptoms.
due to the inability to maintain sufficient caloric intake.
Progressive difficulty breathing (dyspnea) despite medical interventions or oxygen use
Multiple hospitalizations due to respiratory failure, pneumonia, or other complications
Severe pulmonary hypertension or right heart failure (cor pulmonale)
Chronic hypoxia (low blood oxygen levels) that is poorly managed with oxygen therapy
Significant weight loss (>10% of body weight) due to the inability to eat adequately or difficulty swallowing
Non-healing ulcers, wounds, or respiratory infections

Cardiovascular conditions such as congestive heart failure (CHF) or severe arrhythmias

Chronic obstructive pulmonary disease (COPD) or emphysema

Pulmonary fibrosis or other restrictive lung diseases

Neurological disorders that impair respiratory function, such as ALS or other motor neuron diseases
Respiratory function: Arterial blood gas analysis showing severe hypoxemia or hypercapnia
Frequency of hospitalizations: History of multiple acute exacerbations or respiratory failure
Oxygen dependence: Need for supplemental oxygen more than 50% of the day or night
Weight loss: Documented >10% weight loss or inability to maintain nutritional intake due to respiratory distress

End-stage heart disease refers to the final stages of chronic cardiovascular conditions where the heart’s ability to pump blood effectively is severely compromised. Hospice eligibility is determined based on functional decline and complications from the heart disease.

Have a prognosis of six months or less if the disease follows its expected course.
Have this prognosis certified by both the patient’s primary care physician and the hospice medical director.
Choose to discontinue curative treatments in favor of comfort-focused care.
Hospice eligibility may extend beyond six months as long as the patient continues to meet the eligibility criteria.
End-stage heart disease patients may qualify for hospice if they demonstrate:
The patient is unable to carry out any physical activity without severe symptoms, such as dyspnea (shortness of breath), fatigue, or chest pain.
The patient experiences symptoms such as shortness of breath or edema even when at rest.
Despite optimal medical therapy, the patient continues to experience significant symptoms of heart failure such as dyspnea, fatigue, or swelling.
The patient has frequent admissions for heart failure exacerbations or related conditions.

Recurrent hospitalizations for heart failure or cardiovascular complications
Severe edema or fluid retention, requiring frequent management
Pulmonary edema or difficulty breathing even at rest
Significant weight loss or cachexia associated with heart failure
Severe arrhythmias that cannot be controlled with medication or interventions

Chronic kidney disease or dialysis dependence

Severe coronary artery disease

Diabetes mellitus with poor control
Chronic lung disease such as COPD

Stroke or transient ischemic attack (TIA)

Advanced cancer or other life-limiting comorbidities
Ejection fraction: A left ventricular ejection fraction (LVEF) of 20% or less, indicating severe heart failure
Functional status: Severe limitations in activities of daily living (ADLs) such as bathing, dressing, or ambulation
Frequency of hospitalizations: Multiple hospital admissions for heart failure exacerbations or arrhythmias
Weight loss: Documented significant weight loss or cachexia related to the heart disease
Fluid status: Persistent edema or pleural effusion despite diuretic therapy

Patients with severely reduced left ventricular ejection fraction (LVEF) may qualify for hospice when their heart can no longer pump sufficient blood, and they choose comfort-focused care.

Prognosis of six months or less, certified by both the primary physician and the hospice medical director.
Decision to forgo curative treatments.
Continued eligibility if decline persists beyond six months.
LVEF ≤ 20% on recent echocardiogram or cardiac MRI.
NYHA Class IV symptoms—unable to carry out any physical activity without discomfort; symptoms at rest.
Refractory heart failure symptoms despite optimal medical therapy (ACE inhibitors, beta‑blockers, diuretics).

Recurrent hospitalizations for acute decompensated heart failure.
Severe fluid overload (pulmonary or peripheral edema) unresponsive to diuretics.
Cachexia or unintentional weight loss > 10%.
Symptomatic hypotension or syncope related to heart failure.
Arrhythmias (e.g., ventricular tachycardia) requiring frequent interventions.

Renal insufficiency or dialysis dependence.

COPD or other chronic lung disease.

Diabetes mellitus with end‑organ damage.

Coronary artery disease refractory to revascularization.
Ejection fraction report from the most recent imaging study.
Hospital admission records for heart failure exacerbations.
Medication history documenting use of guideline‑directed medical therapy.
Weight trends showing cachexia or fluid shifts.
Functional status assessments (e.g., difficulty with ADLs, bed‑bound status).

Chronic liver disease in its end stage can lead to life-limiting complications. Hospice care focuses on symptom relief and comfort.

Prognosis of six months or less, certified by both the primary physician and the hospice medical director.
Decision to forgo curative treatments.
Continued eligibility if decline persists beyond six months.
Prothrombin time > 5 seconds above control without anticoagulants (INR > 1.5).
Serum albumin < 2.5 g/dL.
Refractory ascites or spontaneous bacterial peritonitis despite treatment.
Hepatorenal syndrome or hepatic encephalopathy unresponsive to therapy.
Recurrent variceal bleeding despite therapy.

Spontaneous bacterial peritonitis (SBP)
Hepatorenal syndrome (elevated creatinine & BUN with oliguria)
Refractory hepatic encephalopathy
Recurrent variceal hemorrhage
Progressive malnutrition or muscle wasting

Active alcoholism (>80 g ethanol/day)

Hepatocellular carcinoma

Hepatitis B or C refractory to therapy
Post–liver transplant (if awaiting transplant, hospice discharge upon organ availability)
Latest INR, albumin, and bilirubin levels
Imaging confirming ascites or variceal bleeding
Records of encephalopathy episodes or SBP
Nutritional assessments (weight loss, muscle mass)

End-stage acute renal failure without intent for dialysis or transplant may be hospice-eligible.
Prognosis ≤ 6 months, certified by physician and hospice medical director.
Patient opts out of dialysis/transplant.
Ongoing eligibility if kidney function continues to decline.
Creatinine clearance < 10 mL/min (< 15 mL/min for diabetics).
Serum creatinine > 8.0 mg/dL (> 6.0 mg/dL for diabetics).
Uremic symptoms: Nausea, vomiting, confusion, pericarditis, GI bleeding, DIC.

Mechanical ventilation requirement
Sepsis or severe infections
Cachexia (weight loss > 10%)
Electrolyte imbalances (e.g., hyperkalemia > 7 mEq/L)

Advanced cardiac or pulmonary disease

Immunosuppression/AIDS
Malignancy
Recent BUN/creatinine trends
Records of electrolyte disturbances
Evidence of uremic complications (pericarditis, coagulopathy)

End-stage acute renal failure without intent for dialysis or transplant may be hospice-eligible.
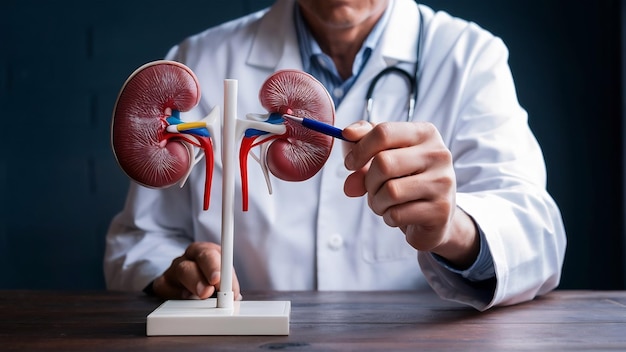
Prognosis ≤ 6 months if untreated, certified by physicians.
Decision against dialysis or transplant.
Re-evaluation if patient’s status changes.
Creatinine clearance < 10 mL/min (< 15 mL/min for diabetics).
Serum creatinine > 8.0 mg/dL (> 6.0 mg/dL for diabetics).
Symptoms of uremia; Fatigue, anorexia, pruritus, fluid overload.

Intractable hyperkalemia (> 7 mEq/L)
Uremic pericarditis
Hepatorenal syndrome
Severe fluid overload unresponsive to therapy

Hyperparathyroidism

Nephrogenic systemic fibrosis

Vascular diseases (e.g., calciphylaxis)
Trends in GFR and creatinine clearance
Evidence of refractory electrolyte imbalances
Records of fluid overload and uremic symptoms

End-stage acute renal failure without intent for dialysis or transplant may be hospice-eligible.

Prognosis ≤ 6 months, certified by physician and hospice medical director.
Decision to forgo aggressive treatments like rehabilitation or surgery.
Eligibility remains if deterioration continues beyond six months.
Severe neurological deficit: Non-ambulatory or unable to perform activities of daily living (ADLs).
End-stage coma or persistent vegetative state.
Severe cognitive impairment, unable to communicate or respond.
Significant weight loss, dehydration, or malnutrition, often linked to dysphagia.

Aspiration pneumonia
Deep vein thrombosis or pulmonary embolism
Sepsis or recurrent infections
Severe spasticity or contractures
Recurrent seizures

Cardiac disease or pulmonary disease

Renal insufficiency

Neurologic decline (e.g., dementia or Alzheimer's progression)
Neurological assessments (e.g., Glasgow Coma Scale, NIHSS)
Dysphagia or feeding issues
Imaging confirming brain injury or infarction
Weight loss or nutritional deficiencies

Patients who are in a persistent coma or vegetative state due to traumatic or non-traumatic causes may qualify for hospice care.

Prognosis ≤ 6 months, certified by physician and hospice medical director.
Decision to forgo curative care.
Eligibility is re-evaluated periodically if condition deteriorates further.
Persistent vegetative state (PVS) or brain death diagnosis.
Absence of purposeful movement or spontaneous respiration.
Inability to communicate (no eye contact or verbal response).

Sepsis
Aspiration pneumonia
Intractable electrolyte imbalances
Recurrent pressure ulcers (stage 3-4)
Multi-organ failure

Traumatic brain injury

Hypoxic-ischemic encephalopathy

Neurological deterioration from another underlying condition
Brain imaging (CT/MRI) confirming coma or vegetative state
Evidence of multi-organ failure or sepsis
Nutritional assessments, including feeding tube use

End-stage HIV/AIDS patients who are non-responsive to treatments or have reached an advanced stage may be eligible for hospice.

Prognosis ≤ 6 months, certified by physician and hospice medical director.
Decision to forgo antiretroviral therapy or aggressive interventions.
Continued eligibility if immunosuppression progresses.
CD4 count 100,000 copies/mL despite treatment.
Progressive weight loss, cachexia, or failure to thrive.
Recurrent opportunistic infections, such as TB, pneumonia, or fungal infections.
Severe neurological impairment, including HIV-associated dementia.

Recurrent infections (e.g., tuberculosis, cytomegalovirus)
Wasting syndrome or unintentional weight loss > 10%
Progressive immunodeficiency
AIDS-related malignancies (e.g., Kaposi’s Sarcoma)

Neurological decline (e.g., HIV encephalopathy, dementia)

Cancer (Kaposi's Sarcoma, lymphoma)

Severe opportunistic infections

Severe coagulopathy or thrombocytopenia
CD4 count, viral load trends
Record of recurrent infections or malignancies
Nutritional assessments and weight loss documentation

Cancer patients with advanced, incurable disease who are no longer responding to curative treatment may qualify for hospice care.

Prognosis ≤ 6 months, certified by physician and hospice medical director.
Decision to discontinue curative treatments like chemotherapy or radiation.
Eligibility re-evaluated periodically if decline continues.
Metastatic cancer with symptomatic progression despite treatment.
Uncontrolled pain, nausea, or vomiting that is not manageable with current therapies.
Weight loss > 10% of body weight over the last 6 months, or BMI < 18.5.
Performance status; Poor performance (e.g., Karnofsky or ECOG scale < 50%).

Bowel obstruction
Severe bleeding
Intractable pain
Sepsis
Liver failure or renal failure
Neurological deterioration due to brain metastases

End-stage organ failure (cardiac, pulmonary, renal)

Chemotherapy side effects (bone marrow suppression, neutropenia)

Inability to maintain weight or fluids
Imaging showing disease progression (e.g., CT/MRI scans)
Pain management charts or palliative care treatments
Weight loss, nutritional support documentation
Performance scale documentation (Karnofsky/ECOG)

At Hospice El Paso, we provide personalized, expert care for your loved ones during life’s most challenging moments. Trust us to guide you with dignity and compassion.